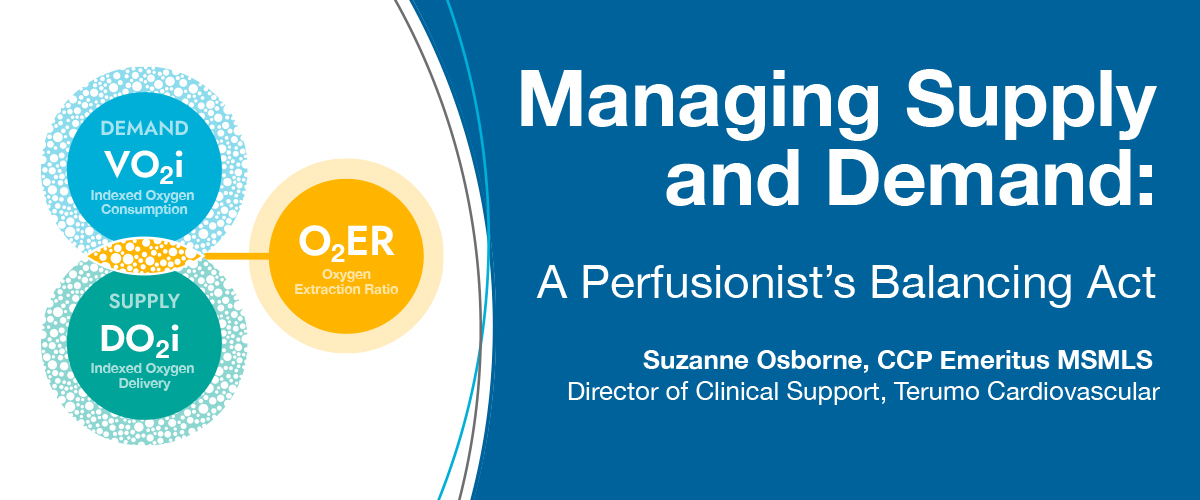
Supply and Demand. The Patient and the Pump. What you’re giving versus what they are using. Perfusionist’s problem or anesthesiologist’s problem? No matter how you ask the question, the answer is “oxygen delivery and oxygen consumption.” Perfusionists need to carefully watch the ratio of oxygen delivery to oxygen consumption— also known as oxygen extraction ratio (O2ER). It is the variable we need to consider when a patient is on cardiopulmonary bypass (CPB) to help us understand the dynamic changes encountered.
We all know the equations from perfusion school: (O2 delivery = 10 x ((1.36 x HGB x SaO2) + (0.0031 x PaO2)) x flow, indexed divided by BSA; O2 consumption (SaO2 - SvO2) x 1.36 x HGB x flow x 10, indexed divided by BSA, and O2 extraction ratio VO2/DO2). We all had to memorize these equations to pass the American Board of Cardiovascular Perfusion exams, but these equations and boundaries have been lost in the daily practice of perfusion. Why? Have we become so device-reliant that we only worry about mechanical alarms such as air, level, and pressure? Are we thinking if we have a “good” cardiac index and a “sufficient” venous saturation, we are perfusing the patient to their needs? This raises a larger question: what should our true goal be as perfusionists? Is it to move the patient safely out of the operating room? To discharge them from the hospital without adverse outcomes? Or is it something more?
"This raises a larger question: what should our true goal be as perfusionists? Is it to move the patient safely out of the operating room? To discharge them from the hospital without adverse outcomes?
Or is it something more?"
Our goal as perfusionists should be optimal care and optimal outcomes through expert CPB management utilizing all the resources or tools available. Goal-directed perfusion is giving the best patient care possible within the operating suite during CPB, using the tools at our disposal. Our tools include advanced equipment, precise equations, clinical data, and close monitoring of the patient’s response. Using all these resources enables the best possible outcomes when our patients walk out of the hospital.
An expert never relies on only two tools to care for a patient. Instead, the clinician should integrate multiple indicators and technologies to provide personalized patient care.
Low oxygen delivery during CPB has been shown by many authors to have adverse outcomes on patients. There have been numerous retrospective studies showing the incidence of acute kidney injury (AKI), the negative impact of prolonged ventilation, increase in hospital cost due to a lower-than-optimal oxygen delivery to end tissues when patients are undergoing CPB.1,2,3,4,5 These studies have varied threshold levels in which they saw the percentage of patients post CPB with AKI. Clinical teams need to look at supply while monitoring oxygen delivery, but the other part of the picture is demand.Demand is oxygen consumption. What your patient requires can vary greatly depending on many factors. Those factors are influenced by anesthesia, age, preoperative status with fluids and drugs, temperature, and by the metabolic rate of the patient.
A patient undergoing CPB will have a different oxygen consumption profile depending on the stage of the procedure. The oxygen consumption of a patient differs from cooling to warming, and from protocol to protocol. Typically, when CPB is initiated, a patient is cooled and their metabolic demands decrease, and the depth of anesthesia is higher. A steady state is reached, and the patient is kept there so the surgical procedure can continue. Next, warming occurs, in which metabolic demands are increased, and a lighter protocol of anesthesia is used. Lastly, weaning and termination of bypass occurs. Oxygen consumption needs to be very closely monitored, and clinical interventions need to occur during all the stages of CPB.
Each of these parameters (DO2i, VO2i, and O2ER) will independently give clinicians a picture of what is occurring in their patient, but the parameters are interdependent and are directly related. Therefore, it is important to look at them together and to consider the ratio in which they influence and interact with each other, and how we can use the ratio to optimize care.

Oxygen extraction ratio is oxygen consumption divided by oxygen delivery. A patient’s normal oxygen extraction ratio during CPB is about 25%, but this number will vary depending on influences in each stage of bypass. By incorporating the oxygen extraction ratio in your practice, you can determine if the patient’s demand is greater than the oxygen supply and could be producing a lactic acid by-product resulting in a metabolic acidosis stage. In your initiation and cooling stage, by examining your oxygen extraction ratio, you can understand if you are safely perfusing your patient in relation to your institutional normal DO2i threshold goals. Institutional DO2i threshold goals may be set at 272 ml/min/m2 or even 300 ml/min/m2, but as a patient is cooled, those goals can be influenced by factors such as cardioplegia dilution and anesthesia protocols. Therefore, incorporating oxygen extraction and oxygen consumption parameters in relation to DO2i enables a clinician to look at each patient independently, and not just a delivery number.
On the flip side, when you are warming the patient and the oxygen extraction ratio is rising from the normal 25%, your institutional norms may be to fast-track a patient. Consequently, your depth of anesthesia is light and the patient is creating lactic acid and experiencing a metabolic acidosis and anaerobic deficit. That anaerobic deficit is not shown by a number above DO2i (supply) threshold—it is indicated by an increase in your oxygen consumption and an increase in your oxygen extraction ratio.
In 2020, Ignacio Condello, PhD, conducted a retrospective study that compared two perfusion strategies—one guided by cardiac index and SvO2 and the other using DO2i and oxygen extraction ratio. In doing so, he reintroduced oxygen extraction ratio to clinical practice and showed clinicians that there is a new, yet familiar, way of creating better patient outcomes. He concluded that by managing indexed DO2 in relation to an oxygen extraction ratio, there is a reduced incidence of hyperlactatemia during surgery, and it can reduce postoperative serum creatinine, mechanical ventilation time, and ICU stay.6
It is imperative that clinicians take a comprehensive approach to goal directed care, carefully examining each parameter and integrating them for context. Ensuring an optimal oxygen extraction ratio and balance is crucial for patient outcomes during bypass.7 Use oxygen extraction ratio to know if you are supplying the correct amount of oxygen for the demand that your patient needs to avoid critical oxygen deficiency, ischemia, and ultimately organ dysfunction.